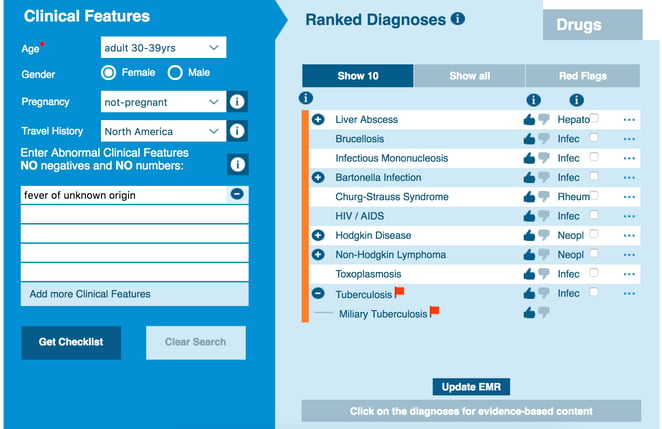
recurrent fever in adults
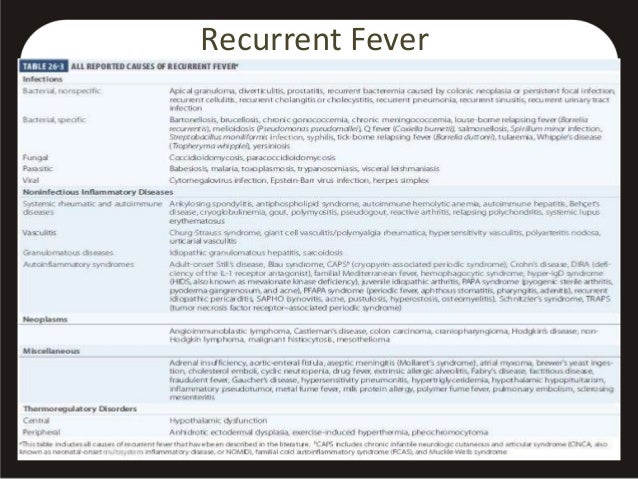
» Pediatrics OVERVIEW regular fever syndromes: What each practitioner needs to know Are you sure your patient has a regular fever syndrome? What are the typical findings of these diseases? Periodic fever syndromes (PFS) are a group of rare auto-inflammatory diseases characterized by inappropriate, uncontrolled and often spontaneous signs and symptoms of inflammation. Recurrent fever ≥ 38°C is the cardinal characteristic in each PFS. Recurrent fever episodes occur in the absence of infection or evidence of active autoimmunity. Fevers in the PFS are due to anomalies in the activation of the innate immune system. Fever and swelling attacks can last days to weeks apart by good health intervals for weeks to months. The pattern of fever (duration and periodicity) and clinical characteristics are variables between syndromes and patients. The associated symptoms usually resolve spontaneously when the patient becomes feverish. However, in severe cases of hereditary disease, inflammation can be chronic with persistent symptoms and the development of long-term complications. The initiation of symptoms is usually in childhood, but may be delayed until adolescence or later. For an individual patient, there is often a predictable pattern of fever, a common constellation of associated symptoms and a similar course of acute disease. Most PFSs are inherited and share the following characteristics: Symptom constellation, including fever pattern, associated symptoms, acute phase response, family history and ethnic origin suggest diagnosis that can be confirmed by genotyping. Significant long-term morbidities and higher mortality occur in untreated patients. Increased risk of illness and secondary amyloidosis in certain ethnic groups. Due to defects of single genes encoding proteins involved in controlling inflammatory pathways, cytokines and apoptosis mediating innate immune responses. Genotipate can guide long-term treatment and prognosis. Hereditary PFS:Mediterranean Fever (FFM)Hyperimmunoglobulinemia DF regular fever syndrome (HIDS)Tumoral (TNF) associated periodic syndrome (TRAPS)Recurrent syndromes associated with cyriopyrin (CAPS):Babym syndrome-Wells (MWS) Multisystem inflammatory disorder (NOMID) Cyccal diseaseCreditant lymphomas, or other chronic infections of the disease PFS is considered auto-inflammatory, not autoimmune, diseases that may or may not have specific triggers. When present, triggers may include cold, heat, stress, surgery, concurrent infection, pregnancy, and vaccines. The clinical manifestations of PFS are due to the inappropriate activation and regulation of antigenoindependent inflammation (innate immunity). Most PFSs are due to defects of unique genes that bind proteins in the path of inflammation control, cytokines production or cell death. What laboratory studies should you ask to help confirm the diagnosis? How should you interpret the results? Bleeding, Bleeding, Bleeding, Bleeding, Bleeding, Bleeding, Bleeding, Bleeding, Bleeding, Bleeding Positive serologies of IgM, PCR or cultures suggest infection. Elevado ACE suggests sarcoidosis. Positive PPD suggests tuberculosis. High uric acid, especially if there is associated leucocytosis or thrombocytopenia, suggests leukemia. ANA ≥1:320, positive lupus serologies, or ANCA suggests a possible systemic autoimmune disease. Hypogammaglobulinemia suggests secondary infection of primary immunodeficiency. Hypergammaglobulinemia suggests HIV or systemic autoimmune disease. Suspectful suspects if IgD is raised with or without IgA elevated and IgG normal and IgM. Would imaging studies be useful? If so, what? Chest X-ray may be useful when infection, lung inflammatory disease, or seroitis (pleuritis, pericarditis) is suspected. Abdominal or ultrasound X-rays may be indicated to evaluate abdominal pain, or to help rule out peritonitis or a surgical emergency. A CT scan of the neck, chest, abdomen, or pelvis may be needed to evaluate lymphadenopathy, lung inflammatory disease, serositis or splenomegaly. The echocardiogram is indicated to evaluate chest pain and rule out pericarditis. Consider the analysis of bone gallon to rule out osteomyelitis. Consider joint RRM with and without contrast for arthritis. Consider magnetic resonance with and without contrast, and MRA to evaluate for CNS vasculitis and causes of headache, developmental delay or hearing loss. Diagnosis ConfirmationPermanent history: Document recurrent fever episodes ≥38°C.FOR at least 4-12 months. No simultaneous infectious symptoms. Fever characteristics: Temperature of peak fever Fever pattern (hectic, quotidian, relapse, relapsing/periodic, continuous, intermittent, sender)Fever durationAntencing or prodrome symptoms before fever startsSymptoms associated (rash, arthritis, diarrhea, etc.) Pattern of symptoms associatedDating of associated symptoms Predictability of symptoms and course of diseaseDating intervals free of fever General health and persistent or chronic symptoms when afebrile Family history of similar fever diseases and response to treatmentEthnicity of parents Number and type of infections in life and response to antibiotics. PFS Suspect Diagnosis If:Recurring ovals without history of infectious symptoms or response to antibiotics. Intervals free of good health fever generally. Family history, especially in the first relative degree, of similar symptomsAmyloidosis, chronic uveitis, hearing loss, serositis or arthritis are also present. If you can confirm that the patient has a regular fever syndrome, what treatment should be started? Therapies to be instituted immediately are shown in Table I. FMF Colchicine 1 mg p.o. daily regardless of age or weight Intravenous fluids as required If significant serositis: consider prednisone 0.5-2 mg/kg/day or methylprednisolone 10-30 mg/kg (max 1 gm) IV times a day 1-3 doses; waist and discontinue with symptomatic improvementEvite unnecessary surgery TRAPS NSAIDs for pain: Naproxen 10 mg/kg b.i.d.; celecoxib 50-100 mg b.i.d.; meloxicam 0.125 mg/kg (max 15 mg) a day; or indomethacin 1 mg/kg b.i.d. Consider prednisone 0.5-2 mg/kg/day for severe symptoms, waist and discontinue with symptomatic improvement or methylprednisolone 10-30 mg/kg (max 1 gm) IV times a day 1-3 days HIDS Avoid unnecessary surgeryNSAIDS for fever or pain: Naproxen 10 mg/kg b.i.d.; celecoxib 50-100 mg b.i.d.; meloxicam 0.125 mg/kg (max 15 mg) daily; or indomethacin 1 mg/kg b.i.d. For severe or NSAID-resistant symptoms: Consider prednisone 0.5-2 mg/kg/day, belt and discontinue with symptomatic improvement or methylprednisolone 10-30 mg/kg (max 1 gm) IV times a day 1-3 days NOMID IL-1 Block: Rilonacept 4.4 mg/kg (max 320 mg) SQ on day 1, then 2.2 mg/kg (max 160 mg) SQ q.wk, ORCanakinumab 150 mg SQ q.8 wk si mento4 andr mg/kg mg daily. 1-3 mg/kg (max 150 mg) SQ q.8 wk if 40 kg are met, ORAnakinmax 1-10 Consider prednisone 0.5-2 mg/kg/day for severe symptoms; waist and discontinue with symptomatic improvement Omeprazole 10-20 mg daily FCAS Cold Avoidance MWS IL-1 Block: Rilonacept 4.4 mg/kg (max 320 mg) SQ on day 1, then 2.2 mg/kg (max 160 mg) SQ q.wk, ORCanakinumab 150 mg SQ q.8 wk if ≤4 yr mg/kg mg daily; 2-3 mg/kg (max 150 mg) SQ q.8 wk if 40 kg are met FPA None Table II lists long-term treatment for periodic fever syndromes. FMF Colchicine 0.3-1.8 mg a day depending on mutation genotyped TRAPS NSAIDS alone for mild symptoms Prednisone 0.5-2 mg/kg/day for chronic symptoms Etanercept 0.4-1 mg/kg (max 25 mg) SQ 2-3 times wk or 0.8-1 mg/kg (max 75 mg) SQ q.wk for severe symptoms HIDS NSAIDSPrednisone 0.25-2 mg/kg/day for symptoms or chronic bursts as needed (often without benefits)IL-1 block: Anakinra 1-2 mg/kg (max 100 mg) SQ daily at the beginning of symptom as necessary or chronically O inhibition of TNF: Etanercept 0.4-1 mg/kg (max 25 mg/kg) SQ 2-3 mg at wk or 0.8 NOMID Continuous block IL-1:Rilonacept 4.4 mg/kg (max 320 mg) SQ on day 1, then 2.2 mg/kg (max 160) mg SQ q.wk ORCanakinumab 150 mg SQ q.8 wk (consign4y " 0.040 kg); 2-3 mg/kg (max 150 mg) SQ q.8 wk (at 40 kg) ORAzobkinra 1 mg per day FCAS Cold avoidance SNAIDS only if minimal symptoms Intermittent or Chronic Block IL-1:Rilonacept 4.4 mg/kg (max 320 mg) SQ on day 1, then 2.2 mg/kg (max 160) mg SQ q.wk ORCanakinumab 150 mg SQ.8 wk (consign4 and " ny 40 kg); 2-3 mg/kg (max. MWS Continuous IL-1 Block:Rilonacept 4.4 mg/kg (max 320 mg) SQ on Day 1, then 2.2 mg/kg (max 160 mg) SQ q.wk ORCanakinumab 150 mg SQ q.8 wk (consign4 and " confidential40 kg); 2-3 mg/kg (max 150 mg) SQ q.8 wk (resulted40 kg) ORAnakinra 1-3.5 FPA No treatmentPrednisone 1-2 mg/kg/day (max 60 mg) times 1-2 days at the beginning of symptoms Consider cimetidine 20-40 mg/kg/dayRespective amigectomy (controversial as first-line treatment) Alternative treatments are listed in Table III if standard therapy fails. FMF IL-1 Block:Anakinra 1-2 mg/kg (max 100 mg) Daily ORCanakinumab 150 mg SQ q.8 wk (conference4 and " √40 kg); 2-3 mg/kg (max 150 mg) SQ q.8 wk (assigned40 kg)Thalidomide 100-300 mg per day if the IL-1 block does not send symptoms TRAPS IL-1 Block: Anakinra 1-2 mg/kg (max 100 mg) Daily block of SQ ORIL-6: Tocilizumab 4-12 mg/kg IV q.2-4 wk HIDS Other IL-1 blockages: Rilonacept 4.4 mg/kg (maximum 320 mg) SQ on day 1, 2.2 mg/kg (maximum 160 mg) SQ q.wk ORCanakinumab 150 mg SQ q.8 wk (maximum concentration of 1 mg/kg maximum weight) 2-3 mg/kg (max. 150 mg) SQ q.8 wk (40 kg) NOMID TNF block: Infliximab 5-10 mg/kg IV q.4-8 wkConsider thalidomide 100-300 mg daily FCAS TNF block: Infliximab 3-7.5 mg/kg IV q.4-8 wk MWS TNF block: Infliximab 3-10 mg/kg IV q.4-8 wk FPA IL-1 intermittent block: Anakinra 1 mg/kg (max 100 mg) SQ within 48 hr of attack startup; can repeat onceCochicina 0.3-1.2 mg dailyTonsillectomy Table IV offers advantages and disadvantages of drug options to treat regular fever syndromes. Drugs Advantages Disadvantages Anakinra IL-1 recombinant antagonist that inhibits the union of IL-1 to IL-1 receptor of the cell surface, thus blocking the activity IL-1 Daily painful injections; short-term effectiveness without long-term benefits after interruption Rilonacept Recombinant IL-1 decoy receptor that binds IL-1 before you can join the receiving cell surface Weekly injections; relatively new without long-term security data Canakinumab Monoclonal Ab to IL-1 that blocks the activity IL-1 Every 8 wk injections; relatively new without long-term security data Etanercept Soluble TNF receiver that binds TNF before it can tie the cell surface receiver Weekly or weekly injections; best long-term safety profile Infliximab Monoclonal Ab to TNFalpha that blocks your activity; long-term security data available Frequent infusion reactions; requires a medical environment to manage; fairly common adverse reactions; known safety data What are the adverse effects associated with each treatment option? Table V gives the adverse effects associated with each treatment option for periodic fever syndromes. NSAIDS Gastritis, gastric ulcer, gastroesophageal reflux, edema, hepatic/renal toxicity rare in children Corticosteroids Infection, weight gain, muscle atrophy, supranocortical insufficiency, osteopenia, growth delay, avascular necrosis, emotional weakness, edema, hypertension, diabetes Colchicine Nausea, vomiting, diarrhea, abdominal pain, anorexia, peripheral neuropathy, muscle weakness, rhabdomiolysis, renal/living toxicity, rash Etanercept Infection, reaction of the injection site, CNS/demyelinating disorder, ANA positivity, malignity (very low risk) Infliximab Infections (several risk), allergic reaction, anaphylaxia, nausea, diarrhea, abdominal pain, fatigue, high LFT, serum disease, ANA positivity, CNS/demyelinating disease, major heart failure, cytopenias, future malignancy (risk etanercept) Anakinra Infection, reaction / pain at the severe injection site, future malignity Rilonacept Infection, reaction of the injection site, hypersensitivity reaction, hyperlipidemia, ? malignant future Canakinumab Infection, reaction at the injection site, diarrhea, nausea, vertigo, weight gain, myalgia, headache, future ills Tocilizumab Infection, thrombocytopenia, allergic reaction, anaphylaxia, CNS/demyelination disorder, GI perforation, elevated LFT, hyperlipidemia, future malignancy Azathioprine Infection, leucopenia, pancitopenia with low methyl-totile transfer activity (TPMT), liver toxicity, nausea, vomiting, secondary malignancy Simvastatin Constipation, dyspepsis, rhabdomiolysis, hepatitis, acute kidney failure Cimetidine Headache, cytopenias Thalidomide Infection, peripheral neuropathy, drowsiness, teratogenicity, eruption, dizziness, mood changes Cyclosporine Infection, hypertension, kidney toxicity, kidney failure, hirsutism, GI disorder, malignancy, CNS toxicity, gynagival hyperplasia Tonsillectomy Pain/risks of surgery What are the possible results of regular fever syndromes? There are some significant morbidities and growing mortality rates observed in patients not treated with inherited PFS syndromes: periodic syndromes associated with cyclopoin, CAPS (FCAS, MWS, NOMID/CINCA): Each of these syndromes is due to a autosomal dominant mutation in a single gene, NLRP3. Phenotypes and complications are different between FCAS, MWS and NOMID, although a significant overlap is observed. Everyone shares a characteristic urtical eruption, but the fever may or may not be present. The most severe disease is seen in NOMID, followed by MWS and FCAS. The 2° amyloidosis frequency is higher in MWS, followed by NOMID and then FCAS. FCAS (fertile cold self-inflammation syndrome): Generally diagnosed at birth or within the first 6 months of life, based on urticary eruption attacks and fever caused by cold exposure and lasting less than 24 hours. These patients usually have a normal life, but 2° amyloidosis occurs in up to 5% of patients. Daily fatigue, headache and myalgia, even without exposure to the cold, contribute to considerable morbidity. MWS (Muckle-Wells syndrome): Characterized by recurrent but unpredictable fever attacks 38.5° C and hives for 1-3 days, although some symptoms may persist. The starting age is often 90%) and the progressive loss of sensorineural hearing (concentr70%) are pathogenic. Since the fever pattern is less predictable than in FCAS, the diagnosis of MWS is often delayed until hearing loss is observed during adolescence. All patients suffer from severe chronic fatigue, which is referred with IL-1 blockage. Abdominal pain and headaches occur in most patients during the fever, but these are not as severe as in the FMF. Arthralgias are more common than chronic arthritis. Recurrent oral aphtase occurs in patients with mento50% during fevers. NOMID/CINCA (inflammatory disease with multiple neonatal connection systems / chronic childhood neurological joint syndrome): This is the most severe form of CAPS, with chronic urticaria with or without a fever noted at birth or in the newborn period. Continuous symptoms and frequent bengales are not necessarily accompanied by fever. Unlike other PFSs, NOMID follows a chronic course with significant complications, general poor prognosis and shortened life if not treated (by IL-1 block therapy). Early diagnosis and treatment with IL-1 inhibition improves quality of life and delays or prevents morbidities. Severe CNS manifestations are observed in 90% of nontreated patients. The epiphysial arthropathy of overcrowding is patonomonic and develops in 30%-60% of patients. Secondary amyloidosis develops in 10%-25% of patients. Other complications vary in severity and age of appearance, but include: ̊ Delay in early growth, delayed puberty Skull abnormalities, frontal head ̊ Progressive loss of sensorineural hearing from early childhood in √70%. Chronic aseptic meningitis, often with chronic headache, papilloma and increased intracranial pressure Mild arthritis in √65%, but 30%-60% develop early chronic inflammation of severe joints with characteristic epiphyseal overgrowth, especially of patellae, with progressive joint contractures and limited mobility ̊ Cognitive effectivity. Chronic intraocular inflammation by 50% manifested by previous uveitis/posterior resistant to treatment, optical atrophy and severe vision loss by 25% or blindness. Hyperimmunoglobulinemia D with regular fever syndrome (HIDS) Attacks can begin in the first year of life with a medium age to an initial attack of 6 m. All patients have their disease at the beginning of 5 years, although the diagnosis is often delayed unless there is a family history of HIDS. Clinical attacks are characterized by non-referent fever ≥ 38.5°C for 3-7 days, in recurrent cycles every 4-8 weeks. Prodrome symptoms such as chills, fatigue, and URI are common. Cervical lymphadenopathy pronounced occurs in √90% and splenomegaly is observed in 50% (distinguishing HIDS from other PFS). Rebounds of severe abdominal pain due to serositis may result in unnecessary exploratory laparotomy or appendicectomy procedures. Non-destructive arthritis or arthralgia occur in 80%. Chronic rashes are observed in Â80% and are variable in appearance. Patients with HIDS usually have a normal life with few serious complications that are not 2° amyloidosis (in family Mediterranean fever (FFFFF)The initial attack of FMF usually occurs in early childhood; 80%-90% are 38° C and abdominal pain for 1-3 days repeating every 3-8 weeks. Patients are asymptomatic and generally good health among attacks. The main cause of mortality is amyloidosis of 2° that leads to kidney failure: Before the cochicin: 2° of amyloidosis occurred in 60%-75% of patients with 40 years of age; in 30% of Sephardic Jews, 60% of Turks; √75% of North African Jews. Country of origin (Turkey, Armenia, Arab nations) and M694V mutation in MEFV gene associated with increased risk of amyloidosis. Some patients have amyloidosis as the first clinical manifestation of the FMF. Continuous colquicine prevents amyloid-related nephropathy in most patients. In the cochicina: 95% improvement, 70% shipping,10%-15% develops amyloidosis 2°. Diagnosis can be confirmed in symptomatic people without identifiable MEFV mutations, if the six-month trial of colchicin remittance attacks is repeated after the suspension of the cochicin. Complications/morbidities include: recurrent peritonitis in 90%, leading to unnecessary abdominal surgery, infertility, recurrent pleuritis intestinal obstruction in 45%; occasionally pericarditis Artritis mono oligo-in 75%. Current aseptical orchidMeningitisErytheme similar to erythema, but rare. Diagnosis in children requires ≥2 of 5 criteria: fever, abdominal pain, chest pain, arthritis and family history of the FFF. Recurrent and unpredictable outbreaks of prolonged fevers √38°C – 41°C, lasting 3 days to 6 weeks, are characterized by tumor necrosis factor (TRAPS)TRAPS. The episodes are repeated on average every 5-6 weeks. The age in the initial presentation is very variable: 50 yr; medium starter age: 3 yr. These patients usually have a normal life, but the previous mortality may be due to a 2° amyloidosis in 10% patients. Other important morbidities include: RashMigratory myalgias monoarticular arthritis, which often precedes fever, are cardinal characteristics Ocular inflammation at 80%Abdominal painTable VI summarizes the risks and benefits of treatment options available for CAPS. Drugs Indicator Risks Benefits NSAIDS Arthritis; pain, fever Adverse reactions Reduce fever, pain, arthritis Corticosteroids Fever, arthritis, serositis, urticaria, vasculitis, lymphdenopathy, organ inflammation/damage Adverse reactions; they can shorten intervals between or increase the frequency of PFAPA attacks by 30%. Relief of fever, rash; improvement of adenopathy, arthritis; lower involvement of organs, serositis Colchicine FMF treatment and possible PFAPA; fever, afty stomatitis, 2° amyloidosis in FMF Adverse reactions; short-term benefit in PFAPA Avoids attacks in √70% and decreases attacks in 95% of the FMF (without effect on TRAPS, HIDS, CAPS); decreases serum amyloids A (SAA) in the FMF; decreases/prevents amyloidosis 2° in the FMF; reduces fever, oral afta; decreases PFAPA recurrences in √50%. Etanercept TRAPS treatment; arthritis, afty stomatitis, fever, 2°amiloidosis and other complications Adverse reactions; they can trigger TRAPS and MAS bengalas Controls fever, arthritis, aftose stomatitis; improves inflammatory markers; lowers SAA; reduces amyloidosis 2° and ? other complications in TRAPS Infliximab Chronic arthritis, fever and inflammation not controlled by etanercept, chronic uveitis, macrophagen activation syndrome (MAS) Adverse reactions; trigger paradoxical TRAPS bengalas Controls fever, arthritis, afty stomatitis, uveitis; improves inflammatory markers; improves the MAS Anakinra CAPS treatment; fever, hives, rash, arthritis, high ESR/CRP; MAS and some FMF, HIDS and TRAPS do not respond to conventional therapy, consider for FPAPA. Adverse reactions; triggers the appearance of inflammation; not control of long-term diseases outside treatment Remits fever, rash, arthritis and laboratory abnormalities in FCAS, MWS (less effective in NOMID) and some FMF, HIDS, TRAPS, FPAPA; low SAA; reduces amyloidosis 2° and other complications in CAPS; remit MAS. Rilonacept CAPS treatment; fever, rash, arthritis, laboratory anomalies Adverse reactions; Remit fever, rash, arthritis, and lab abnormalities in many patients with CAPS Canakinumab Colchicin-resistant CAPS and FF treatment; fever, rash, arthritis, laboratory anomalies Adverse reactions Complete referral in 95% CAP patients; normalizes SAA; reduces 2° amyloidosis and other long-term complications in CAPS Tocilizumab TRAPS treatment does not respond to etanercept or anakinra; arthritis, elevated ESR/CRP Adverse reactions Standardizes CRP, ESR and SAA; effect on 2° unknown amyloidosis Azathioprine HIDS resistant to standard therapy Adverse reactions It can reduce symptoms of HIDS in some patients Cyclosporine HIDS resistant to standard therapy Adverse reactions It can reduce symptoms and episodes of HIDS in some patients Thalidomide Treatment of NOMID, TRAPS, FMF resistant to standard therapy; arthritis, afty stomatitis Adverse reactions You can reduce ESR/CRP in some patients with HIDS Simvastatin HIDS resistant to standard therapy Adverse reactions; may trigger HIDS bengalls It can reduce HIDS episodes in some patients What causes this disease and how often is it? Epidemiology: FMF: Most common hereditary PFS. Predominantly affects people living in the Mediterranean region. Incidence: 1-3/105 in Turkey, Armenia, North Africa, Arab countries and Italy; rare in other places. Clinical symptoms and the range/frequency of individual mutations in Arabs differ from other ethnic groups and vary according to the country of birth. Carrier Rate: 1:3 – 1:7 in Jews, Armenians and Turks in North Africa and Iraqis who have serious illnesses and increase amyloidosis. 1:5 in Ashkenazi Jews, but the prevalence of diseases is lower, since the most common mutation is associated with mild disease. Thin male predominance (13:10). TRAPS:Incidence: rare (5-6/107 person-yr in Germans). Many of the Scottish or Irish ancestors; as a result, initially called Fiebre Hiberniano Familial. It affects women and men alike. HIDS:Incidence: Very rare (frequency of the 1:350 mutation in the secondary Holland to the founding effect. Conf.60% of the Dutch or French descent and generally Caucasian. Men and women equally affected. FCAS: Many of the European ancestry. Incidence: very rare. MWS: Most reported in Europe and North America, but limited data from other areas. Incidence: rare, generally familiar. Equally affected men and women. NOMID:Most of those reported frequently in Europe and North America, but limited data from other areas. Incidence: rare. Less likely FCAS or MWS are family members. Genetics: FMF: autosomal recessive mutations (homozygous or composite heterocigous) (conejército 50) in the MEFV gene encoding pyrin/marenostrin. Four mutations of evidence in exon 10 (M680I, M694V, M694J and V726A) and E148Q in exon 2 represent most mutations. All mutations decrease the function of pirin30% of symptomatic patients, including mandatory carriers, have only one identifiable MEFV mutation. Diagnosis should never be excluded on the basis of genetic tests only if clinical characteristics are observed. The M694V mutation is more common, confers greater gravity and risk of amyloidosis and predominates in Jews, Armenians and Turks from North Africa and Iraqi. In the Jews of Ashkenazi, the most common mutations (V726A and E148Q) have reduced penetration and conferred a milder phenotype of disease. TRAPS: autosomal dominant mutations in TNFRSF1A genes that used the 55 kDa TNF receptor with incomplete disease penetration. ratio mutations almost exclusively affect the extracellular part of the TNF receptor. Many patients with TNFRSF1A clinical characteristics have not identified TNFRSF1A mutations. HIDS: Homozygous or heterocigous compound mutations in mevalonated kinase (MVK) gen encoding mevalonate kinase. 80% carry at least one V377I mutation. mutations. CAPS (FCAS, MWS, NOMID): dominant autosomal (gain) mutations in the NLRP3 (CIASI) cryptopyrin/NLRP3.10% FCAS, 25% MWS and 30%-50% NOMID/CINCA lacks NLRP3 identification mutations. Inflammatory and Innate Immunity The distinctive seal of innate immunity is the rapid generation and release of pro-inflammatory cytokines, including IL-1beta, TNF-alpha and IL-6, in response to "danger signs" as microbial products, toxins and metabolic stress. Il-1 beta is the pleiotropic pyrogen and the alarm cytokine. Its activation triggers a waterfall of events that result in inflammation and production of other pro-inflammatory cytokines. Activation of the multiprotein intracellular complex called "inflammatory" by signs of danger in neutrophils, macrophages, dendritics and other cells is essential for the release of bioactive IL-1 and the initiation of inflammation. Inflammasome is composed of NLRP3, cocoa-1 and ASC (apoptosis-associated) protein similar to that of mota). Inflammatory stimulation activates the hose-1, which converts IL-1beta to its bioactive form. Mutations in one or more of the proteins that include inflammatory and subsequent effects on IL-1beta activity have been shown to cause inherited fever syndromes on a regular basis. How do these pathogens/genes/exhibitions cause the disease? CAPS (FCAS, MWS, NOMID): NLRP3 required for the assembly of a multiprotein or "inflammatory" complex in phagocytic cells, monocytes, macrophages, dendrite cells and condrocytes that link the initial detection of the danger of microbial products and metabolic stress to the activation of the innate immune system through the production of the IL-1beta alarm cytokine.Considered "inrinsic inflammasomopathies" – diseases resulting from the growing secretion. Function mutations in NLRP3 cause the activation of the constitutive inflammatory and increase the activity of the hose-1, resulting in excessive release of IL-1beta, uncontrolled inflammation and tissue injury. FMF: The FMF is considered an extrinsic "inflammasomopathy". The pirin plays an intrinsic role in regulating the function of granulocyte and monocyte during inflammatory responses. Pyrin interacts with ASC and disrupts NLRP3-ASC interactions, which inhibits NF-kappa Activation B and apoptosis. The abduction of ASC by pirin prevents the activation of caspase-1. Operating Loss MEFV mutations decrease pirin binding to ASC, which leads to inflammatory activation and increases IL-1beta secretion. Colchicin inhibits neutrophil chemotaxis through the depolymerization of microtubules and reduces the production of pro-inflammatory cytokines through the inhibition of NF-kappaB activation. HIDS: Mevalonated kinase (MVK) is necessary for cholesterol synthesis. MVK catalyzes the conversion of mevalonic acid to 5-phospho-mevalonic acid in the isoprenoid pathway. Severe mutations of loss of functions with absent MVK activity cause mevalonic aciduria, an innate error of metabolism associated with developmental delay and early death. Less severe mutations (known 60) with residual MVK activity of 1%-15% cause HIDS. Etiology of high serum IgD and also IgA (in ю70%) recurrent fevers of decreased MVK activity not fully understood, but includes increased inflammatory activation and overproduction IL-1beta. TRAPS: The soluble TNF cell surface and receptors unite the pro-inflammatory cytokine, TNF, with opposite effects on signaling TNF receptors and TNF secretion during inflammatory responses. Some mutations affect the coating of receptors, allowing sustained stimulation of membrane TNF receptors and lower availability of TNF soluble receptors (short extracellular portions) that work to inhibit more TNF signaling. Most mutations affect the folding and traffic of TNR receptors to the cell membrane, leading to intracellular accumulation of mutant receptors that spontaneously induce the activation of protein kinase in several inflammatory pathways. Other mutations decrease TNF binding to the ligated membrane receptor, inhibiting TNF-dependent apoptosis pathways involved in the control of inflammation. Other clinical manifestations that could help with diagnosis and managementAmyloidosis secondaria in hereditary PFS: Medical management focused on the prevention of 2° amyloidosis. Development of highly variable amyloidosis between different PFSs, but always devastating. Aloid deposition in the kidneys in 90% of patients and usually presents as proteinuria without kidney failure. Kidney failure due to amyloidosis can be the first symptom of the disease. Proteinuria in disease presentation or with follow-up requires a 24-hour urine collection for the cleaning of proteins and creatinine. Amyloidosis diagnosed by kidney or rectum biopsy. Consider renal and/or rectal biopsy if the protein √500 mg in 24-hour urine collection or BUN/creatinine elevation. Average survival time: 2453 m from the time of diagnosis without treatment. Amyloidosis in the GI tract in 20% patients; it presents as diarrhea and malabsorption. Heart involvement of 2° amyloidosis due to chronic inflammation is rare, unlike other types of amyloidosis. The level of amyloid serum A (SAA) may reflect active amyloid deposition and guidance therapy. Cooking prevents renal amyloidosis in the FMF, but not in HIDS, TRAPS or CAPS. Genotype: phenotype correlations and controversies that affect treatment decisions in FMF:Homozygous patients for M694V mutation or composite heterozygous for M694V and other disease-causing mutation (V726A-E148Q) should initiate chronic cochicin therapy as soon as the diagnosis confirmed by genotyped. Patients homozygous for V726A-E148Q or composite heterozygous for V726A-E148Q and other disease-causing mutation (not M694V) should receive colchicin at the beginning of attacks and not necessarily chronic cochicin unless severe inflammation, proteinuria or amiodosis occurs. Patients without M694V or V726A-E148Q mutations and mild symptoms may not need colchicin unless the attacks are severe or develop amyloidosis, which would be unlikely. Diagnosis and treatment with colchicin should not be excluded in individuals with typical clinical symptoms that lack identifiable MEFV mutation. What complications can you expect from disease or treatment of the disease? Most self-limited complications, but some affect health and quality of life, including unnecessary abdominal surgery and secondary infertility to pelvic adhesions, as well as unique morbidities to NOMID. The complication of the most worrying disease is amyloidosis of 2°, which is the main cause of morbidity and mortality. Treatment complications can be more common than those of the disease, including the worsening of inflammation, organ toxicity, infection and future malignancy. Are there additional laboratory studies available; even some that are not widely available? Serum amyloid A protein (SAA) urinary mevalonic acid level TNF receptor level How can PFS be prevented? No known prevention. Genetic counselling is suspected to be important if PFS is inherited. Prenatal diagnosis requires identification of disease-causing mutations. Masters, SL, Simon, A, Aksentijevich, Kastner, DL. "Horror autoinflammaticus: the molecular physiology of auto-inflammatory disease". Ann Rev Immunol. vol. 27. 2009. pp. 621-68. Bodar, EJ, Drenth, JP, van der Meer, JW, Simon, A. "Deregulation of innate immunity: hereditary syndromes of regular fever." Brit J Haematol. vol. 144. 2008. pp. 279-302. Simon, A, van der Meer, JW. "Patogenesis of family fever syndromes or hereditary auto-inflammatory syndromes". Am J Physiol Regul Integr Comp Physiol. vol. 292. 2007. pp. R86-98. Kastner, DL, Aksentijevich, A, Goldbach-Mansky, R. "Recharged auto-inflammatory disease: a clinical perspective." Cell. vol. 140. 2010. pp. 784-90. Ombrello, MJ, Kastner, DL. "Auto-inflammation in 2010: expansion of the clinical spectrum and expansion of the therapeutic horizons." Nat Rev Rheumatol. vol. 7. 2011. pp. 82-4. Henderson, C, Goldbach-Mansky, R. "Self-inflammatory monogenic diseases: new ideas on clinical aspects and pathogenesis". Curr Opin Rheumatol. vol. 22. 2010. pp. 567-78. van der Hilst, JC, Simon, A, Drenth, JP. "Regular hereditary fever and reactive amyloidosis." Clin Exp Med. vol. 5. 2005. pp. 87-98. Bilginer, Y, Akpolat, T, Ozen, S. "Real amyloidosis in children". Pediatr Nephrol. vol. 26. 2011. pp. 1215-27. Glaser, RL, Goldbach-Mansky, R. "The specter of monogenic auto-inflammatory syndromes: understanding of the mechanisms of disease and use of specific therapies." Curr Allergy Asthma Rep. vol. 8. 2008. pp. 288-98. Goldbach-Mansky, Kastner, DL. "Auto-inflammation: the prominent role of IL-1 in monogenic auto-inflammatory diseases and the implications for common diseases." J Allergy Clin Immunol. vol. 124. 2009. pp. 1141-9. McDermott, MF, Aksentijevich, I, Galon, J. "German mutations in the extracellular domains of the 55 kDa TNF receptor, TNFR1, defines a family of dominant inherited auto-inflammatory syndromes." Cell. vol. 97. 1999. pp. 133-44. Hull, KM, Drewe, E, Aksentijevich, I. "The periodic syndrome associated with the TNF receptor (TRAPS): emerging concepts of an auto-inflammatory disorder." Medicine (Baltimore). vol. 81. pp. 349-68. Rezaei, N. "TNF-receptor-asociated periodic syndrome (TRAPS): an autosomal dominant multisystem disorder". Clin Rheumatol. vol. 25. 2006. pp. 773-7. Vaitla, PM, Radford, PM, Tighe, PJ. "Role of interleukin-6 in a patient with tumor necrosis factor receptor-associated periodic syndrome: evaluation of results after treatment with the monoclonal antibody of the anti-interleukin-6 tocilizumab receptor." Arthritis Rheum. vol. 63. 2011. pp. 1151-5. Pettersson, T, Kantonen, J, Matikainen, S, Repo, H. "TraPS Settings". Ann Med. vol. 44. 2012. pp. 109-18. Samuels, J, Ozen, S. "Family Mediterranean fever and the other autoinflammatory syndrome: patient assessment with recurrent fever." Curr Opin Rheumatol. vol. 18. 2006. pp. 108-17. Chae, JJ, Aksentijevich, I, Kastner, DL. "Advances in understanding family Mediterranean fever and selective fever possibilities". Br J Haematol. vol. 146. 2009. pp. 467-78. Goldfinger, SE. "Cochicina for the family's Mediterranean fever." New Engl J Med. vol. 287. 1972. pp. 1302Shohat, M, Halpern, GJ, Pagon, RA, Bird, TD, Dolan, CR. "Familial Mediterranean fever". 1993-2000 Aug 08. Ozen, S, Bilginer, Y, Aktay Ayaz, N, Calguneri, M. "Anti-interleucina 1 treatment for patients with family-run colchicin-resistant Mediterranean fever." J Rheumatol. vol. 38. 2011. pp. 516-8. van der Hilst, JC, Bodar, EJ, Barron, KS. "International HIDS Study Group. Long-term follow-up, clinical characteristics and quality of life in a series of 103 patients with hyperimmunoglobulinemia D syndrome." Medicine (Baltimore). vol. 87. 2008. pp. 301-10. van der Hilst, Frenkel, J. "Hyperimmunoglobulin D Syndrome in childhood". Curr Rheumatol Rep. vol. 12. 2010. pp. 101-7. Korppi, M, van Gijn, ME, Antila, K. "Hyperimmunoglobulinemia D and regular fever syndrome in children. Revision of therapy with biological drugs and case report." Acta Paediatr. vol. 100. 2011. pp. 21-5. Haas, D, Hoffmann, GF. "Mevalonated kinase deficiency and auto-inflammatory disorders." N Engl J Med. vol. 356. 2007. pp. 2671-3. (CAPS):Mitroulis, M, Skendros, P, Ritis, K. "Targeting IL-1beta in disease; the expanding role of NLRP3 inflammasome". Eur J Intern Med. vol. 21. 2010. pp. 157-63. Kubota, T, Koike, R. "Recurrent syndromes associated with crysopyrin: background and therapeutic." Mod Rheumatol. vol. 20. 2010. pp. 213-21. Aganna, E, Martinon, F, Hawkins, PN. "Association of mutations in the NALP3/CIAS1/PYPAF1 gene with a broad phenotype that includes recurrent fever, cold sensitivity, sensorineural deafness, and AA amyloidosis." Arthritis Rheum. vol. 46. pp. 2002. 2445-52. Lepore, L, Paloni, G, Caorsi, R. "Following and quality of life of patients with periodic syndrome associated with cryoperin treated with Anakinra." J Pediatr. vol. 157. 2010. pp. 310-15. Church, LD, McDermott, MF. "Canakinumab: a human anti-IL-1β monoclonal antibody for the treatment of periodic syndromes associated with cryoperin." Expert Rev Clin Immunol. vol. 6. 2010. pp. 831-41. Kuemmerle-Deschner, JB, Tyrrell, PN, Koetter, I. "Anakinra therapy effectiveness and safety in pediatric patients and adults with Muckle-Wells auto-inflammatory syndrome." Arthritis Rheum. vol. 63. 2011. pp. 840-9. Neven, B, Marvillet, I, Terrada, C. "Long-term performance of interleukin-1 receptor antagonist anakine in ten patients with inflammatory neonatal adjustment multisystem/neurologic, cutaneous and chronic childhood joint syndrome". Arthritis Rheum. vol. 62. 2010. pp. 258-67. Continuous discussions with regard to etiology, diagnosis, treatment Long-term risks/benefits of treatment with biologics, given uncertainties of future risks, especially for malignant neoplasms, opportunistic infections, autoimmune diseases, organ toxicity. Best PFAPA management: steroids vs tonsillectomy vs IL-1 blockage vs non-treatment. Use of colchicin for treatment or prophylaxis in patients with FMF with a non-M694mutation identified or mild presentation. The role of pharmacogenomy in managing regular fever syndromes. Consensus for the treatment of HIDS since conventional immunosuppression is rarely beneficial, most patients do well over time, and may not need chronic biological therapy. Pharmacological options for managing CAPS given difficulty distinguishing between syndromes in some patients, and therefore long-term prognosis. Copyright © 2017, 2013 Decision Support in Medicine, LLC. All rights reserved. No sponsor or advertiser has participated, approved or paid for the content provided by the LLC Medical Decision Support. The Licensed Content is copyrighted by DSM. You got an account yet? Log in CancerTerapyAdvisor.com is a free online resource that offers oncological health professionals a comprehensive knowledge base of practical oncological information and clinical tools to help make the right decisions for their patients. Our mission is to provide practice-centred clinical and drug information that reflects the current and emerging care principles that help inform oncology decisions. Copyright © 2021 Haymarket Media, Inc. All Rights Reserved This material cannot be published, transmitted, rewritten or redistributed in any form without prior authorization. Your use of this website constitutes the acceptance of Haymarket Media and .
:max_bytes(150000):strip_icc()/when-to-see-a-doctor-for-a-fever-770768_FINAL-5c05c20ec9e77c0001e07722.png)
This Is When to See a Doctor for Your Fever

Approach to the Adult Patient with Fever of Unknown Origin - American Family Physician

Approach to recurrent fever in childhood | The College of Family Physicians of Canada

Prolonged Febrile Illness and Fever of Unknown Origin in Adults - American Family Physician

Intermittent fever - Wikipedia
SURFS Disease Info Card 2016 2 - Systemic Autoinflammatory Disease (SAID) Support

Fever, fever patterns and diseases called 'fever' – A review - ScienceDirect

Prolonged and recurrent fevers in children - Journal of Infection

Prolonged Febrile Illness and Fever of Unknown Origin in Adults - American Family Physician
1 Minute Read: Types of Fever Differential Diagnosis
My Child, or I Keep Getting Fevers. What Do I Do? - Systemic Autoinflammatory Disease (SAID) Support
/1719431-article-infections-that-cause-headache-and-fever1-5a7e09acd8fdd50037ee6e81.png)
Infections That Cause Headaches and a Fever
Fever and Abdominal Pain - Infectious Disease and Antimicrobial Agents

Unexplained recurrent fever: when is autoinflammation the explanation? - Kallinich - 2013 - Allergy - Wiley Online Library

Fever in Adults: Characteristics, Types, and When It's Serious
How to Use the Comparison Chart of Systemic Autoinflammatory Diseases Diagnostic Chart

Prolonged and recurrent fevers in children - ScienceDirect

Table 1 from Recurrent Fever of Unknown Origin (FUO) Due to Periodic Fever, Aphthous Stomatititis, Pharyngitis and Adenitis (FAPA) Syndrome in an Adult | Semantic Scholar

Recurrent rheumatic fever in adults. | Annals of the Rheumatic Diseases

Mysterious Fevers and Pain? You May Have Autoinflammatory Disease – Health Essentials from Cleveland Clinic

Fever in Adults: Characteristics, Types, and When It's Serious
Periodic Fever Syndromes in Adults - Systemic Autoinflammatory Disease (SAID) Support

Canakinumab for the Treatment of Autoinflammatory Recurrent Fever Syndromes | NEJM
Fever of unknown origin

COVID-19-Associated Suspected Myocarditis as the Etiology for Recurrent and Protracted Fever in an Otherwise Healthy Adult - The American Journal of the Medical Sciences
Relapsing Fever - Causes, Symptoms, Complications, Diagnosis & Treatment
Persistent low grade fever: Causes and treatments

PDF) Recurrent rheumatic fever

A diagnostic approach to recurrent myalgia and rhabdomyolysis in children | Archives of Disease in Childhood

Fever: 102 Temperature, Severe, Causes, Treatment, Symptoms & Home Remedies
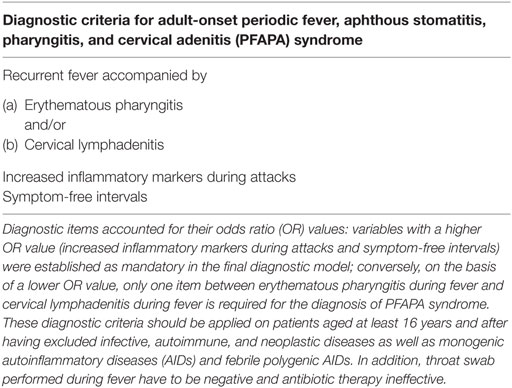
Frontiers | Diagnostic Criteria for Adult-Onset Periodic Fever, Aphthous Stomatitis, Pharyngitis, and Cervical Adenitis (PFAPA) Syndrome | Immunology

Unexplained recurrent fever: when is autoinflammation the explanation? - Kallinich - 2013 - Allergy - Wiley Online Library
COVID-19 and Fever - Together

Prolonged and recurrent fevers in children - ScienceDirect

Prolonged Febrile Illness and Fever of Unknown Origin in Adults - American Family Physician

Pin on Health
Recurrent Fever Syndromes – Queensland Rheumatology Services

CAPS: Cryopyrin-associated periodic syndromes - Symptoms & Causes
Rigante
What is a Periodic Fever Syndrome? - Systemic Autoinflammatory Disease (SAID) Support
Posting Komentar untuk "recurrent fever in adults"